
- ClinicMind customer support
Flexible solutions for your practice, without sacrificing process efficiency.
Wherever and whenever you work, remote access and live support when you need it.
Simplify your path to a thriving practice.
Customize your experience by effortlessly switching between cloud, client-server, and back as you see fit.
Comprehensive software solutions to support billing teams through the entire revenue cycle.
Speak to a real person right away.
Access our secure cloud platform conveniently from any internet-connected device.
Enhance your patient experience with MyClinicMind patient portal.
All-In-One Bolt-On Platform
ClinicMind Mobile EHR
Provider Enrollments Quick & Simplified!
Fully Customizable Reporting
20+ Years Of Medical Billing And Coding Experience
Comprehensive software solutions to support billing teams through the entire revenue cycle.
MyClinicMind Mobile App
Prior Authorization Process
Reclaim Your Time
Bulletproof Joins ClinicMind
Experience the unparalleled efficiency of FlexNote
ClinicMind Offers A Range Of Powerful Integrations
A Division of ClinicMind
Medical Billing Services That Solve Your Collections Headaches
Customize your experience by effortlessly switching between cloud, client-server, and back as you see fit.
Comprehensive software solutions to support billing teams through the entire revenue cycle.
Speak to a real person right away.
Access our secure cloud platform conveniently from any internet-connected device.
Enhance your patient experience with MyClinicMind patient portal.
All-In-One Bolt-On Platform
ClinicMind Mobile EHR
Provider Enrollments Quick & Simplified!
Fully Customizable Reporting
20+ Years Of Medical Billing And Coding Experience
Comprehensive software solutions to support billing teams through the entire revenue cycle.
MyClinicMind Mobile App
Prior Authorization Process
You see what we see. No secrets or surprises.
Tailored training and dedicated coaching for your practice's...
Evolving software for your practice with innovative,...
Speak to a real person right away.
ClinicMind is committed to system compliance, and we proudly hold ONC certification.
The people, processes, and technology to help you reach your goals.
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.

Go-live in as little as 30 days.
Experience top-tier support and training to elevate your journey with us.
Executing a proven success plan together.
Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Continuous learning, excellence, teamwork.
Elevate your career from the comfort of home.
Structure for work-life balance and professional growth.
Discover tools and insights for a profitable, patient-focused practice.
Uniting top minds from across the globe to empower providers to excel.
Meet our leaders in health tech and fintech, driving our client's success.
Our reputable partners: a testament to our software's growing acclaim.
Discover tools and insights for a profitable, patient-focused practice.
Uniting top minds from across the globe to empower providers to excel.
Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Stay ahead with our ONC-certified solutions compliant with the latest healthcare regulations.
Explore books by our leaders, condensing 20+ years of industry knowledge for healthcare leaders like you.
Trace the evolution of industry insights through our articles to empower professionals like you.
Explore the evolution of ClinicMind's innovations for professionals like you.
Explore our blog, committed to enriching the provider journey with expert insights.
Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Drawing from Armenia's rich talent to bolster provider performance.
Mobilizing India's top tech minds to advance provider solutions.
Amplifying provider capabilities with exceptional talent from the Philippines.
Boosting providers with elite U.S. medical billing experts and fintech veterans.
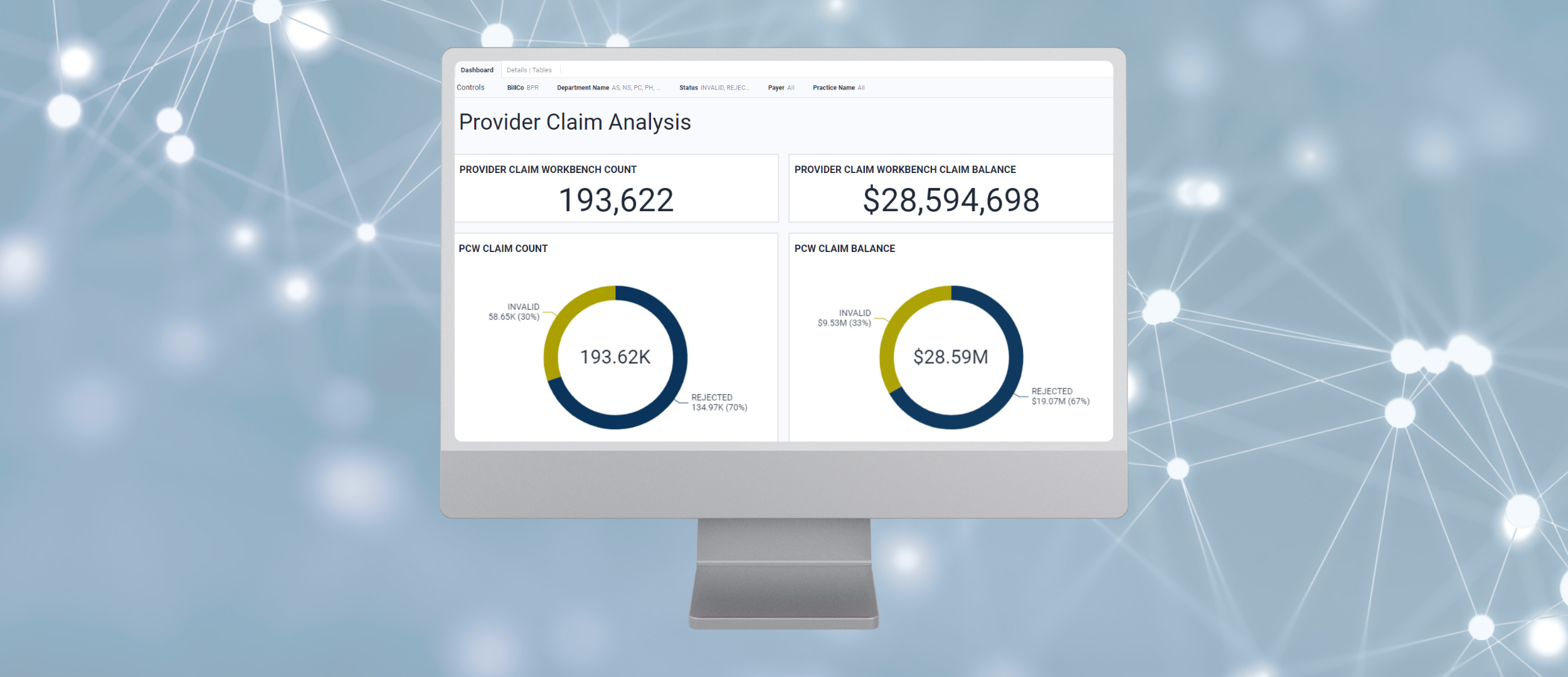
Comprehensive software solutions to support billing teams through the entire revenue cycle.

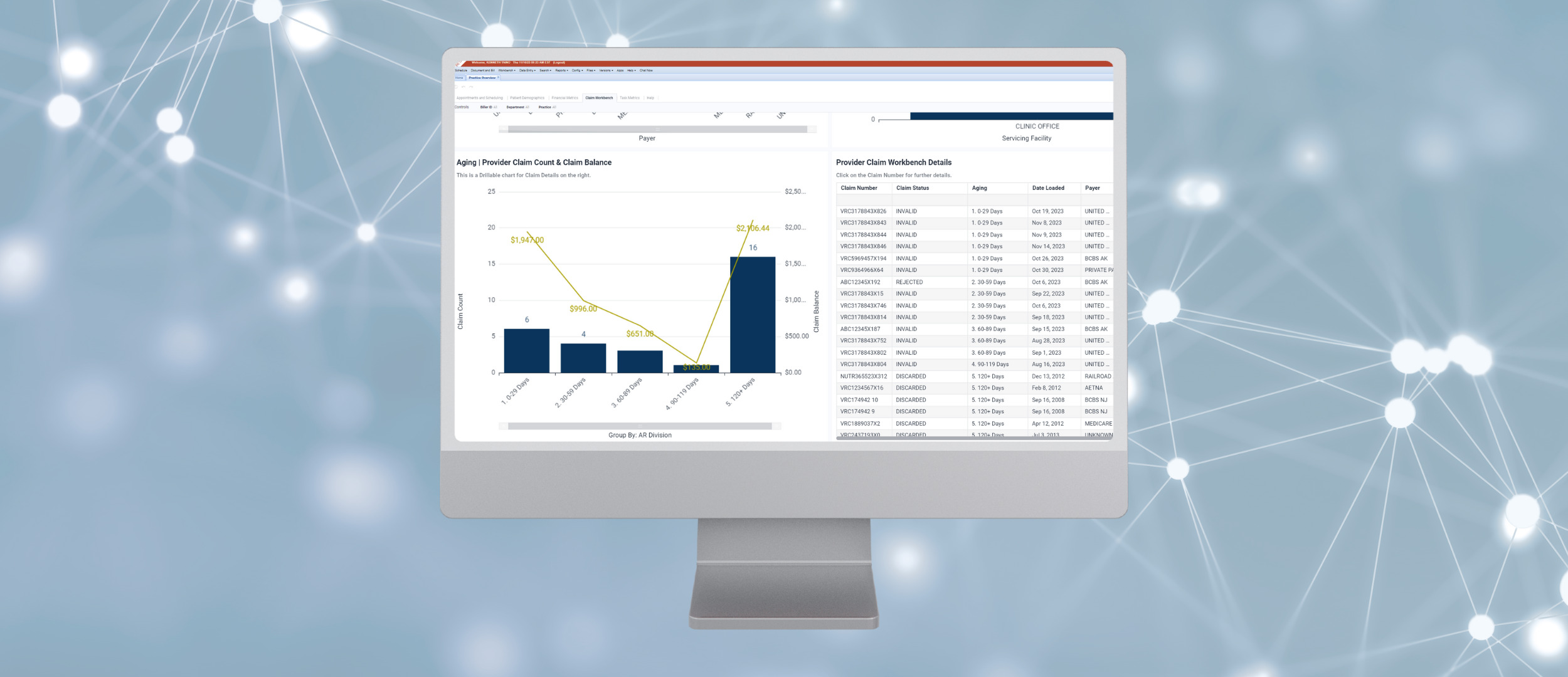
The system helps support billers by tracking the status of all claims and provides an easy platform to submit claims and follow-up directly with the appropriate parties.
Sophisticated billing technology solutions and AI technology that were typically only available to large organizations are now easily accessible by practices of all sizes with ClincMind.

Comprehensive software solutions to support in-house billing teams through the entire revenue cycle. The solution is designed to help billers and providers simplify the billing process and maximize their revenue.
The system helps support billers by tracking the status of all claims and provides an easy platform to submit claims and follow-up directly with the appropriate parties.
Sophisticated billing technology solutions and AI technology that were typically only available to large organizations are now easily accessible by practices of all sizes with ClincMind.
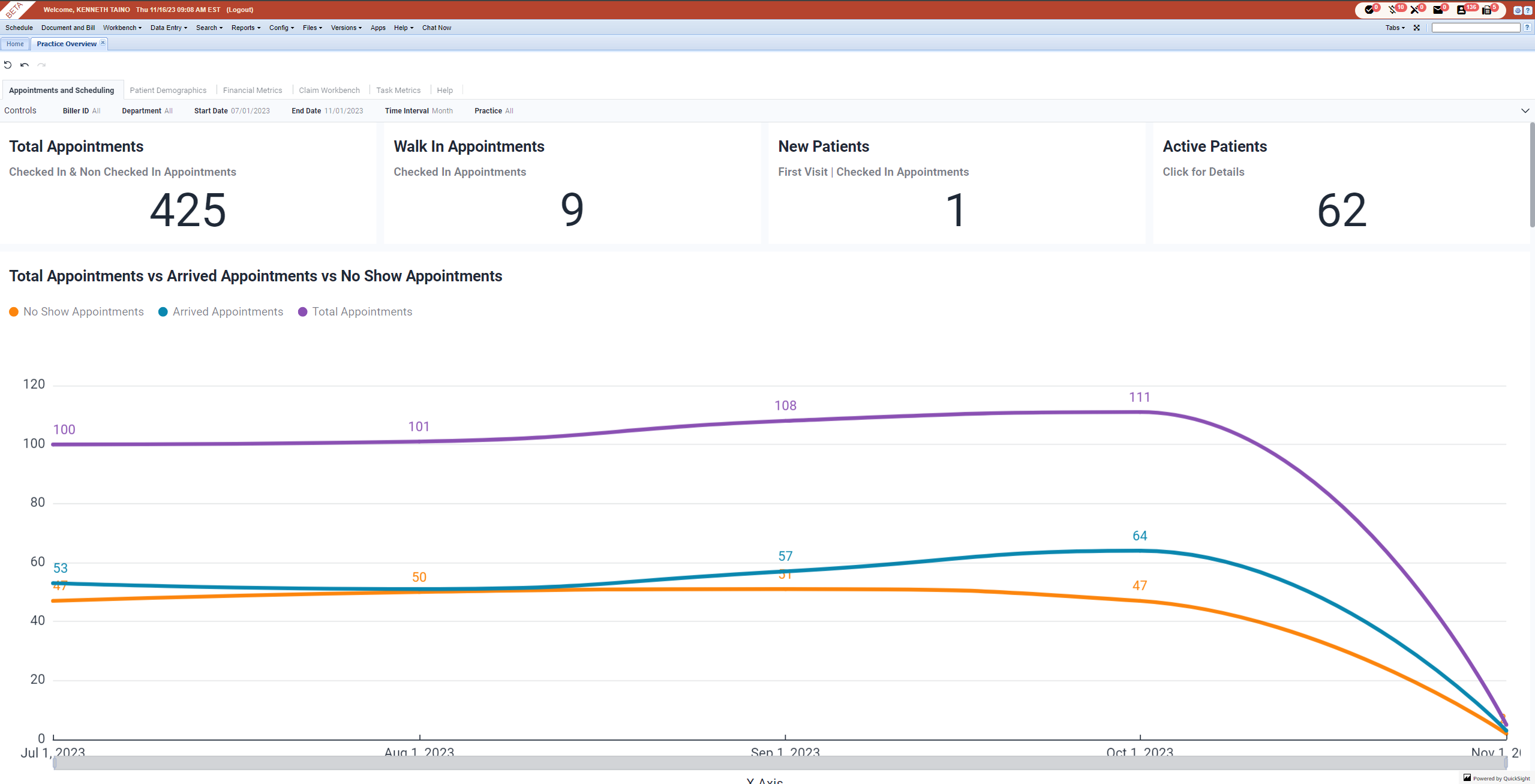
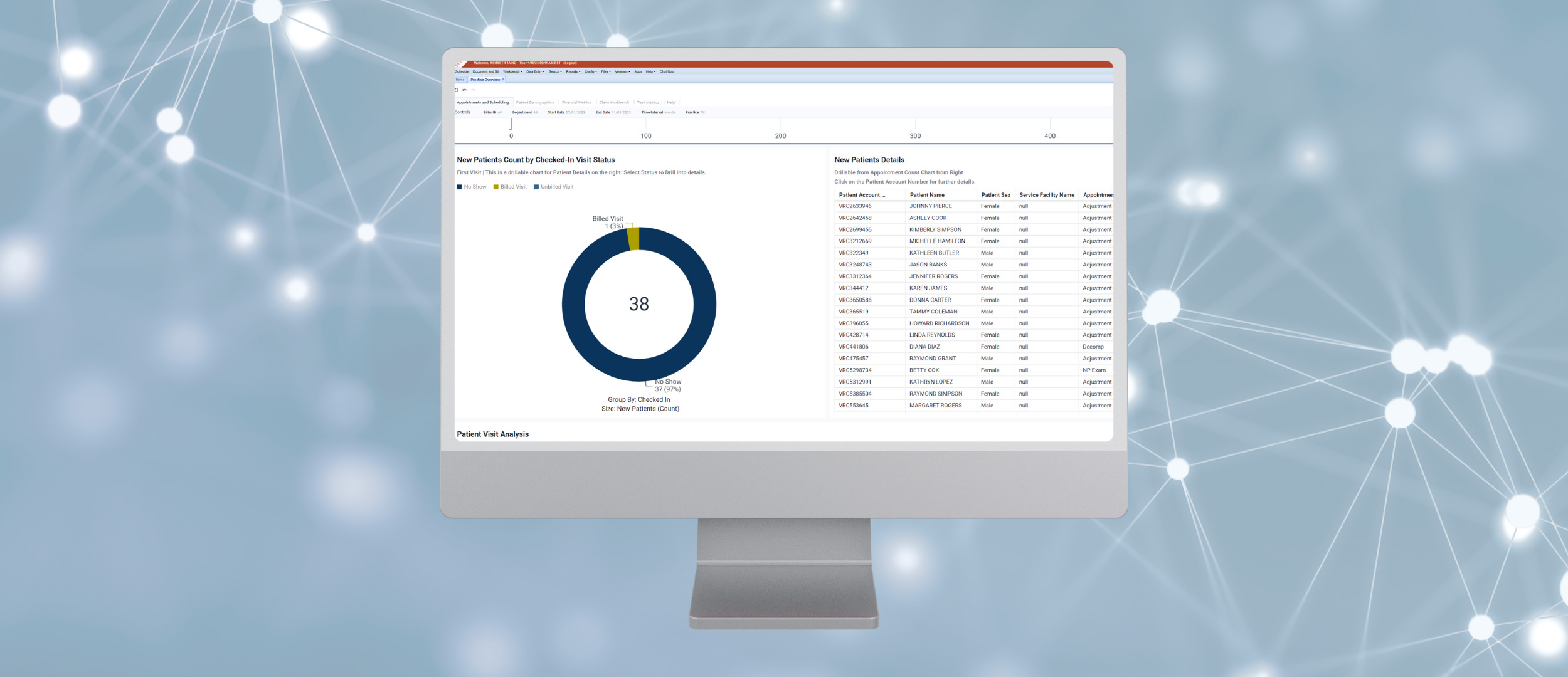
Billing transparency is a top priority at ClinicMind, and we are committed to providing you with easy access to claim details and comprehensive reporting. With our intuitive system, you no longer have to jump from portal to portal to find answers. Our centralized platform consolidates all claim information in one place, allowing you to quickly and easily access the details you need.
We offer over 50 reports that provide transparent insights into your billing operations. These reports cover various aspects, such as tracking revenue, monitoring unbilled claims, patient balances, reconciliation, and more. Our interactive reports store data securely, ensuring that historical financial details are readily available whenever you need them. With ClinicMind, you can say goodbye to time-consuming research and effortlessly access the information you require.
Our system maintains detailed logs that cannot be edited or deleted. These logs provide an accurate and comprehensive record of all billing activities, ensuring accountability and transparency. You can confidently track claims activity, review clearinghouse responses and access payer determination details. With ClinicMind, you have complete visibility into the lifecycle of each claim, empowering you to make informed decisions and effectively manage your revenue cycle.



Developed with data from over 72 million claims, our system scrubs claims against pre-built rules and all known rejection reasons to allow you to fix claims before they are even submitted to reduce back and forth with insurance companies and get you paid faster.

Verify Insurance in real-time.

View actions and status of individual claims or groups of claims.
Yes. Our team will work with you to get your data imported into our system. They will tell you exactly what you need to do.
Some practices choose to process outstanding claims in their previous system and some choose to transfer them to our system.
We are a healthcare technology company empowering providers and managed service organizations to help more patients and grow. Our solutions span clinic operations software and revenue cycle management services
Is a top priority at ClinicMind, and we are committed to providing you with easy access to claim details and comprehensive reporting. With our intuitive system, you no longer have to jump from portal to portal to find answers. Our centralized platform consolidates all claim information in one place, allowing you to quickly and easily access the details you need.
We offer over 50 reports that provide transparent insights into your billing operations. These reports cover various aspects, such as tracking revenue, monitoring unbilled claims, patient balances, reconciliation, and more. Our interactive reports store data securely, ensuring that historical financial details are readily available whenever you need them. With ClinicMind, you can say goodbye to time-consuming research and effortlessly access the information you require.
Our system maintains detailed logs that cannot be edited or deleted. These logs provide an accurate and comprehensive record of all billing activities, ensuring accountability and transparency. You can confidently track claims activity, review clearinghouse responses and access payer determination details. With ClinicMind, you have complete visibility into the lifecycle of each claim, empowering you to make informed decisions and effectively manage your revenue cycle.
ClinicMind is powered by cloud-based software, ensuring a seamless experience for your practice. Here’s what it means for you:
Our software is hosted securely on cloud servers, eliminating the need for individual installations on your computers or servers. This setup offers numerous advantages, including transparent releases and automatic updates.
Software updates occur effortlessly in the background, without disrupting your workflow. You won’t even notice when updates happen, keeping your software equipped with the latest features, enhancements, and security patches.
In the unlikely event of an issue arising from an update, our system seamlessly rolls back to the previous version. This rollback is executed automatically, without causing any disruption to your service. We prioritize a smooth operation for your practice, even in the face of unexpected challenges.
Furthermore, ClinicMind’s cloud-based infrastructure utilizes multiple servers, ensuring near-zero downtime. Even during rare server issues or maintenance activities, our redundant servers maintain your practice’s operational efficiency.
With ClinicMind’s cloud-based software, you gain a reliable solution that is continuously available. Transparent releases, automatic updates, and robust server infrastructure work together to minimize downtime, keeping your practice running smoothly.